- Your cart is empty
- Continue Shopping
All About Polycystic Ovary Syndrome (PCOS)
- PCOS
- Posted on
-
by Dr. Ruhi Agarwala

What is Polycystic Ovary Syndrome (PCOS) ?
PCOS or Polycystic Ovarian Syndrome is a lifestyle disorder that most commonly affects women of reproductive age. It is often misled, because it creates a label that it can’t be cured and can lead to a hopeless feeling.
Generally what needs to be treated is the root cause instead of putting on band-aids that only cover things up. Most women with PCOS have insulin resistance. Insulin resistance is one underlying root cause of PCOS.
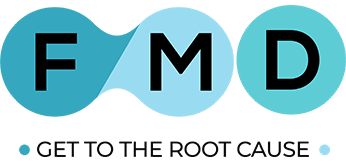
PCOS has various symptoms. Women may have 4-5 of these symptoms.
Common symptoms of PCOS include:
- Acne
- Weight gain or trouble losing weight.
- Extra hair on the face and body. Often women get thicker, darker facial hair and excess hair on the chest, belly, and back.
- Thinning hair on the scalp.
- Mood swings, depression.
- Bloating.
- Irregular periods. Women with PCOS have fewer than nine periods a year. Some women have no periods whereas others have very heavy bleeding.
- Fertility problems. Many women who have PCOS have trouble conceiving.
Struggling with Unwanted Facial Hair and Male Pattern Balding?
One of the symptoms of PCOS can be unwanted facial and body hair growth and male pattern balding. Let’s understand what causes it.
- Most PCOS cycles can be anovulatory cycles
Anovulation leads to higher levels of testosterone. When a woman does not ovulate, the brain is still trying to stimulate that ovulation. Under this stimulation, more and more luteinizing hormones are released. When the ovaries are overwhelmed with luteinizing hormone, they tend to produce significantly higher levels of testosterone. - Testosterone is a male hormone
High levels of testosterone contributes to increase in body hair in women, in particular, on the face, maybe on the nipples or around the belly button area. - High dihydrotestosterone or DHT
High testosterone can also lead to high levels of dihydrotestosterone or DHT which can contribute to loss of head hair in women just like it does in men. - High insulin levels make androgen receptors more sensitive to androgens
Insulin resistance makes androgen receptors more sensitive to androgens and hence the symptoms of balding and unwanted hair growth appear when the Testing for testosterone and DHEAS is essential if you are experiencing the above symptoms. PCOS test covers these parameters.
In Addition, Also Read – How Does Hair Mineral and Toxins Analysis Test Guide You For a Personalized Nutrition Plan?
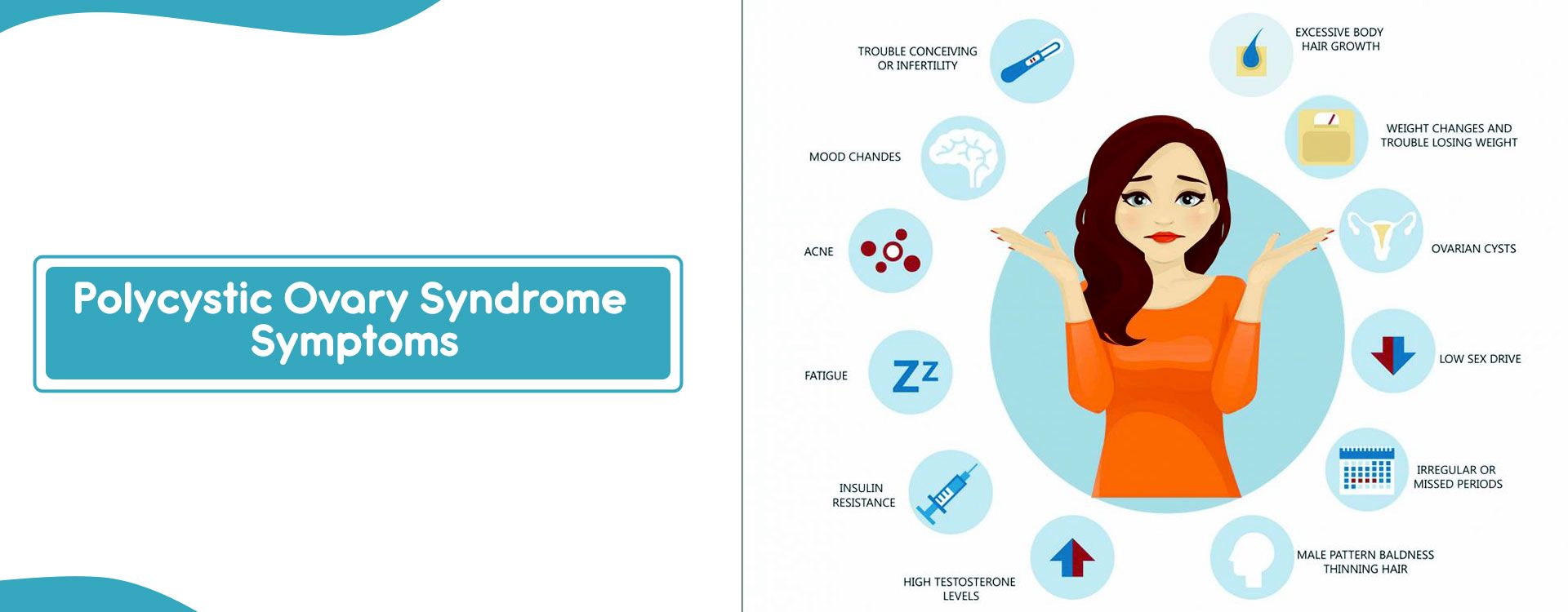
It is not Necessary to Have Cysts in Your Ovaries to Confirm PCOS
Often women get very concerned about having cysts in the ovary. Let’s understand more about the cysts in the ovary.
What does Cysts in The Ovary Mean?
- All women of reproductive age have some ovarian cysts. They’re really quite normal. Ovarian cysts are formed at every attempt at ovulation. The corpus luteum is a normal cyst that forms in the ovary every single month in women of childbearing age after ovulation. Those cysts generally are quite small and they are self-resolving.
- Having some small ovarian cysts is not a problem.
It just means that the reproductive process is happening naturally. - Large cysts accompanied with symptoms of hormonal imbalance need to be addressed
Now larger cysts may arise. They can be painful just because they are causing physical impingement, but again, most often, they are self-resolving. In some cases, they do need to be removed if they are simply growing out of control.
What Causes Large Cysts in The Ovary?
It’s a sign of ovaries that are not generally producing eggs or ovulating consistently. Basically, what’s happening is that the egg maturity process is impaired so that the follicles are trying to mature, but they are not able to finish the maturation process in order to allow ovulation. What someone ends up with is a lot of cysts as evidence of that attempt at maturation, but those cysts are not proceeding to ovulation because the eggs within them are underdeveloped.
Not all women with PCOS will have cysts in their ovaries. Polycystic ovary is only a sign of PCOS and not the cause. You may have a normal ovary along with the symptoms of PCOS.
Main Root Causes of PCOS
Research today clearly points out that there are many different contributing causal factors for PCOS. Two primary drivers for PCOS are:
- Insulin resistance
High circulating levels of insulin, it’s called insulin-resistance. It is the starting point of the metabolic cascade that eventually leads to Type 2 diabetes. 50% of women with PCOS have excess body fat and high waist to hip ratios which are really classic dynamics of insulin-mediated fat storage. So, checking fasting insulin levels is very important. - Estrogen dominance
The second driver is endocrine disruption and subsequent damage to the egg due to hormone-mimicking chemicals or what is often called xenoestrogenic toxicity
Well, I am sure you would be intrigued to know what’s causing Insulin resistance & Estrogen dominance. Here it is in a nut shell.
- Poor diet-Refined carbohydrates/sugar/trans fats
- Nutritional deficiency
- Food sensitivities-gluten, dairy
- Increased Gut permeability
- Imbalance in Gut
- microbiome/Dysbiosis
- Malabsorption
- Chronic stress
- Non Native EMF
- Toxin Load (heavy metals, plastics, personal care products, etc
- Poor Detoxification-Constipation,etc
- Sedentary lifestyle
- Estrogen mimicking foods-dairy & meat fed with hormones, hybrid soya
- Human Genome
References:-
- Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. (2004, January 1). ScienceDirect.
- Dunaif, A. (1997). Insulin Resistance and the Polycystic Ovary Syndrome: Mechanism and Implications for Pathogenesis. Endocrine Reviews, 18(6), 774–800. https://doi.org/10.1210/er.18.6.774
- Pelusi B, Gambineri A, Pasquali R. Type 2 diabetes and the polycystic ovary syndrome. Minerva Ginecol. 2004 Feb;56(1):41-51. PMID: 14973409.
- Diamanti-Kandarakis E., Bourguignon, J. P., Giudice, L. C., Hauser, R., Prins, G. S., Soto, A. M., Zoeller, R. T., & Gore, A. C. (2009). Endocrine-Disrupting Chemicals: An Endocrine Society Scientific Statement. Endocrine Reviews, 30(4), 293–342. https://doi.org/10.1210/er.2009-0002
- De Leo V, Musacchio MC, Morgante G, La Marca A, Petraglia F. Polycystic ovary syndrome and type 2 diabetes mellitus. Minerva Ginecol. 2004 Feb;56(1):53-62. PMID: 14973410.